Will there be a second wave of COVID-19 in the fall? Individuals and organizations are making plans that depend on an answer to that question, and there is much comment in the media to the effect that there definitely will be a second wave. However, specific predictions have limited credibility, due to the poor performance of epidemiological and statistical models in forecasting the progress of the first wave while we are still in it.
Still, we can review some points that bear on the question, both pro and con:
Pro Second Wave
- History’s lessons. The other major pandemics of the 20th century have all had multiple waves. The 1918 “Spanish” flu pandemic, which killed tens of millions of people around the world, had three waves, the second of which was the most deadly. Figure 1 shows these three waves for the UK.
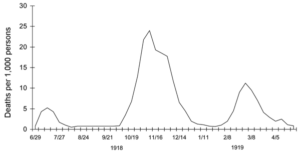
Figure 1. Spanish Flu Pandemic, UK (source: CDC)
The 1957-58 pandemic also had two waves and, as with the Spanish flu, the second wave was worse than the first. The 1968 flu pandemic, likewise, came in two waves, with the first wave more severe in North America, and the second wave more severe in Europe and Asia.
- Large remaining susceptible population – Asymptomatic rates are quite high – greater than 50% – so some have speculated that the virus may already have penetrated much of the population, denying it fertile ground for future growth. However, several antibody surveys taken during the current Covid-19 pandemic show large majorities of the population remain uninfected – a large survey in Spain, which has a higher COVID death rate than the U.S., showed only 5% of the population had antibodies to the virus. (This survey was done in early May, so some increase in antibody exposure is expected, but Spain was well past its peak death rate at that point.)
The aggressive worldwide lockdown substantially suppressed the spread of COVID, bolstering the view that there remains a large susceptible population. The three earlier pandemics referenced were allowed to run their course without lockdowns on the scale we are seeing now, and, even so, they all had multiple waves. - Aggressive virus – COVID-19 is highly infectious, with an R0 that is probably in excess of 2, on a par with that of the Spanish flu. This means that, unimpeded, every case of COVID infects two new people. A virus will die out on its own – hit “herd immunity” – once the remaining susceptible population drops below a certain level, 1-1/R0. The higher R0 is, the more people have to be immune for the virus to die out. By most estimates, herd immunity level for COVID is over 50%, and anything below that will allow subsequent waves. We are nowhere near that level now.
Con Second Wave
- Global reach – Everywhere has been touched by COVID, ensuring that there are few “pockets” of fertile ground ready to launch secondary waves (though there are still large reservoirs of susceptible people, even in hard-hit countries).
- Global knowledge and public health infrastructure – Scientific knowledge is deeper and more widely available today, and global information and coordination about surveillance and mitigation is more widespread. We have the examples of Taiwan and New Zealand to look to, where the initial wave was stifled at birth. COVID infections are especially prone to clustering; in the U.S. over a third of deaths are in nursing homes. An active surveillance and targeted counter-measure protocol should be able to respond to clustered outbreaks.
- Vaccines and therapeutics – There are now hundreds of clinical trials involving potential vaccines and therapeutics, and NIH’s infectious disease chief, Anthony Fauci, has expressed hopes that a vaccine will arrive by January 2021. This might be too late to stop a Fall second wave, but could diminish its full impact.
- Age profile – The age profile for COVID is much more heavily skewed to the old and infirm than it was for the earlier pandemics. This target population is less mobile, and more easily isolated. On the other hand, the population of elderly and infirm is much greater today than in 1918, and more vulnerable generally.
- History – WWI and antibiotics – The 1918 Spanish flu pandemic remains the most ominous historical precedent for second wave mayhem. But, in addition to the age profile there are two important differences between then and now:
-
- WWI was just ending, with millions of troops being demobilized and returning home. Young men, who were quite susceptible to that H1N1 strain of the flu, were traveling from all over Europe to everywhere in the world.
- Most of the serious cases eventually involved bacterial infections, and antibiotics were not available in 1918.
Wild Card
The weather is a wild card. Influenza-like illnesses in the past have always been winter phenomena, dying out in the summer. Is this due to heat? Humidity? Simply the ability to get outdoors? In any case, the current explosive growth of COVID in two enormous tropical countries, Brazil and India, suggests that a shutdown due to summer might not be in the cards. If COVID infections are not responsive to weather, this could mean the “wave” phenomenon of earlier pandemics will be weaker.
Conclusion
History and the large remaining susceptible population favor a second wave. The clustering behavior of the virus and a capable public health infrastructure provide opportunities for escape. The key may be social cohesiveness, especially in the U.S. Suppressing a significant second wave in 2020 without bringing back widespread coercive lockdowns will require a long-term ability to respond rapidly and intelligently to clusters of outbreaks at a hyper-local level. This decentralized, technical approach is difficult to sustain effectively in a polarized civic landscape, where response to COVID becomes entangled with politics.

